Introduction
Delirium is an acute disorder of brain function that is caused by other medical conditions, substance intoxication or withdrawal, or exposure to a toxin. It is characterised by a disturbance in attention, a reduced level of orientation to the environment and other cognitive disturbances that cannot otherwise be explained by neurocognitive disorders.1 Delirium can be regarded as a clinical expression of acute encephalopathy.2 Delirium frequently occurs in hospitalised adults, and is associated with significantly increased ICU and hospital length of stay, mortality, as well as an increased risk of long-term cognitive disorders and loss of independence.3 The economic impact of delirium is substantial. Delirium in older hospitalised adults has been estimated to cost between $38 billion and $152 billion per year.4
For healthcare providers, the large variety in clinical phenotypes and fluctuating clinical course of the syndrome makes screening for and diagnosing delirium notoriously difficult. Furthermore, there is no curative treatment, and the efficacy of both pharmacologic and non-pharmacologic interventions to suppress delirium symptoms is limited.5 Healthcare providers have several practice guidelines, including those published by the American Geriatrics Society and the Society of Critical Care Medicine (SCCM).5,6 There are also guidelines for specific patient groups. Examples include the guideline for postoperative delirium from the European Society of Anaesthesiology.7 Although these guidelines all clearly state how and when patients should be screened for signs and symptoms of delirium, and what potential underlying causes of delirium are, none of the guidelines provides a framework for a structured approach to detection and management of underlying causes or follow-up once delirium is diagnosed.
There are several mnemonics and acronyms that aim to support healthcare providers in detecting the underlying cause of delirium. Examples include “I WATCH DEATH” and “DELIRIOUS”. However, mnemonics and acronyms often do not distinguish for what population they are intended, when and how to use the information they provide, and who developed the mnemonic.(ICU Delirium.Org, retrieved Aug 4, 2023) They also make no distinction between rare and common underlying causes of delirium, or suggest what priority should be given to the individual items.
The prevention, monitoring and treatment of delirium receives an increasing amount of attention. This is due to several factors, including evidence-based practice initiatives like SCCM’s ICU Liberation Project, as well as the arrival of simplified electroencephalography (EEG) devices that can assist in detecting the underlying EEG changes that are seen in acute encephalopathies underlying delirium.8,9 These innovations increase the demand for a structured framework on how to approach patients who are diagnosed with possible delirium.
This paper describes an initiative to create a clinical algorithm to provide healthcare providers with a structured approach to hospitalised patients who develop delirium.
Methods
In December 2020, the initiators of this project (TO, CH and AJCS) convened for the first time to discuss the existing gap in guidance for healthcare providers caring for hospitalised patients with delirium. We outlined a simple, stepwise “template algorithm” that emphasised a structured approach to detecting underlying causes of delirium, followed by suggestions for symptomatic treatments and follow-up. Model content was based on international delirium guidelines5,7,8 systematic reviews on underlying causes and triggers of delirium10,11 and mnemonics found in diverse sources (see table 1).12 We followed a modified Delphi approach to reach expert consensus on the contents of this model, referred to as “the Delirium Delphi Algorithms”.
With attention to diversity in training, gender and nationality, we invited a group of experts to form the interdisciplinary consensus panel. We invited 38 experts to participate. Because of the COVID-19 pandemic, the consensus process took place online. Panel members were presented with concept versions of the algorithms and were asked to respond to design elements (such as the order in which suggestions were presented), text statements (such as: All patients should receive preventive non-pharmacologic measures, regardless of their cognitive state) and could comment on specific textual content. Responses were gathered dichotomously (agree/disagree) and in full-text comments. The online consensus process allowed the Panel members to comment and vote privately, at their own pace.
After each voting round, the responses and comments of the Panel were discussed within the Board. The agreement between Panel members with each design choice, statement or other item offered for voting was calculated by dividing the number of members who agreed by the number of respondents to that particular voting round. Before the start of data collection, we agreed that 85% of agreement needed to be reached within the panel before a statement or design element would be consolidated in the algorithm. Elements or statements with a lower agreement level were adjusted using comments from panel members. The updated version of the algorithm was then offered to the Panel in a new voting round. Items that already reached a high level of agreement were not offered for voting again.
A report with the agreement levels and a motivation for each proposed adjustment to the algorithms was sent to the Panel members before the next voting round.
Results
In total, 38 experts agreed to participate; 37 completed at least one voting assignment (response rate 97%). TO, CH and AJCS acted as a board. Panel members had a background in anaesthesiology (5), cardiac surgery (1), geriatrics (9), intensive care medicine (7), neurology (5), nursing (4), pharmacy (1) and psychiatry and psychology (6) and practice their profession in the United States of America, Australia, Austria, Belgium, Canada, Denmark, Germany, Italy, The Netherlands, Poland, and the United Kingdom (Supplementary Material). All panel members signed the digital participation agreement before completing the first voting assignment. The voting rounds took place between June 2021 and January 2023. The panel required five voting rounds to reach consensus about the set of algorithms (Table 2).
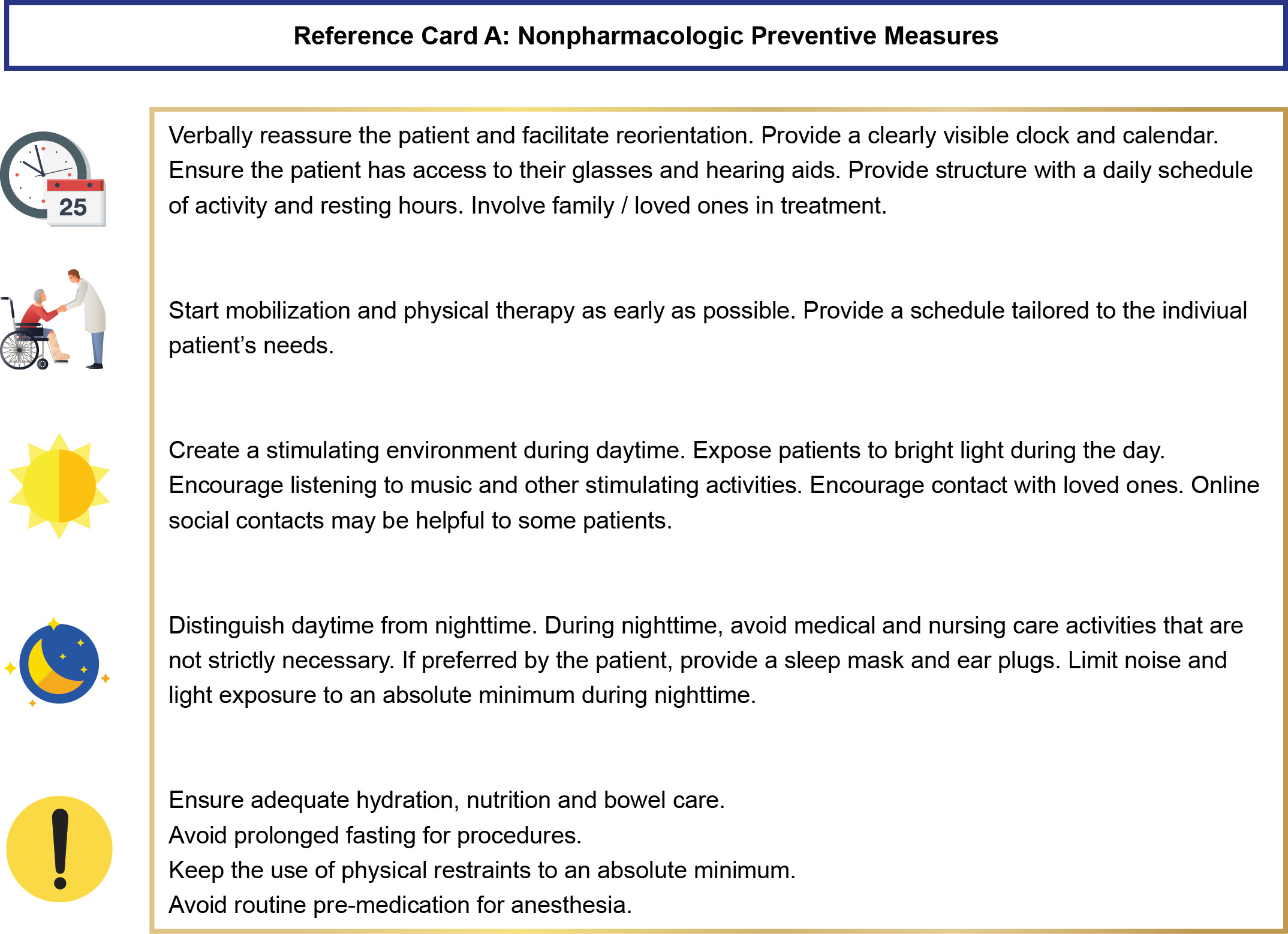
The final product of this process is a set of three algorithms: one for patients in hospital wards, one for patients after cardiac surgery, and one for patients in intensive care units. To improve usability, the content of the algorithms was kept concise. The algorithms share a set of five “reference cards”, which contain more detailed information, such as suggestions for non-pharmacologic interventions. The full set of three algorithms and 5 reference cards, as well as an instruction for users, is presented in the Additional File 2. As an example, the algorithm version for patients in normal hospital wards is shown in Figure 1a. The reference card for non-pharmacologic interventions is presented in Figure 1b.
A detailed record of the modified Delphi voting process is presented in Additional File 1.
Discussion
Using a modified Delphi approach, we developed a set of algorithms to support healthcare providers who take care of hospitalised adult patients with delirium. In five online voting rounds, consensus was reached between a diverse group of 37 internationally recognised delirium experts.
Position relative to guidelines
The Delirium Delphi Algorithms intend to provide structure and prioritisation, and strongly focus on identifying modifiable precipitating factors. As such, these are intended to be used as a tool, in addition to national and international guidelines. The content is primarily based on expert opinion and should be regarded as such. Users are advised to take their local situation into account and always comply with local legislation, particularly when it comes to involuntary medical treatments such as the use of restraints.
Knowledge gap
There is currently no high-quality evidence available to support one particular approach to management of delirium and its underlying causes. The application of the Delirium Delphi Algorithms implies a bundle of several “good clinical practices”. These include structured application of non-pharmacologic interventions to prevent delirium, a strong focus on the identification of modifiable precipitating factors, and follow-up that consists of frequent reassessment of the patient’s need for symptomatic drug treatments. Bundles of interventions have repeatedly been proven to be more effective in reducing the delirium burden than standalone interventions.13
Future of delirium management
With the arrival of innovations in delirium screening and monitoring as well as individualised interventional treatments, the field of delirium management is likely to change significantly in the next ten years. The algorithms will be kept up to date by the authors to follow these developments. We encourage healthcare providers who regularly treat patients with delirium to form interdisciplinary working groups in their institution to keep their delirium management strategies up-to-date.
Conclusion
We present a set of algorithms to support healthcare providers caring for hospitalised adult patients with delirium.
Funding
This project has not received funding.
Disclosures
The authors have no conflicts of interest to disclose.